CRISPR in the Tumor Microenvironment: From Diagnostic Profiling to Precision Therapy
Keywords:
Biomarkers, CRISPR-Cas , Tumor microenvironment, Drug resistance, Gene editing, Targeting therapies, Precision oncology, Oncogenic signaling pathwaysAbstract
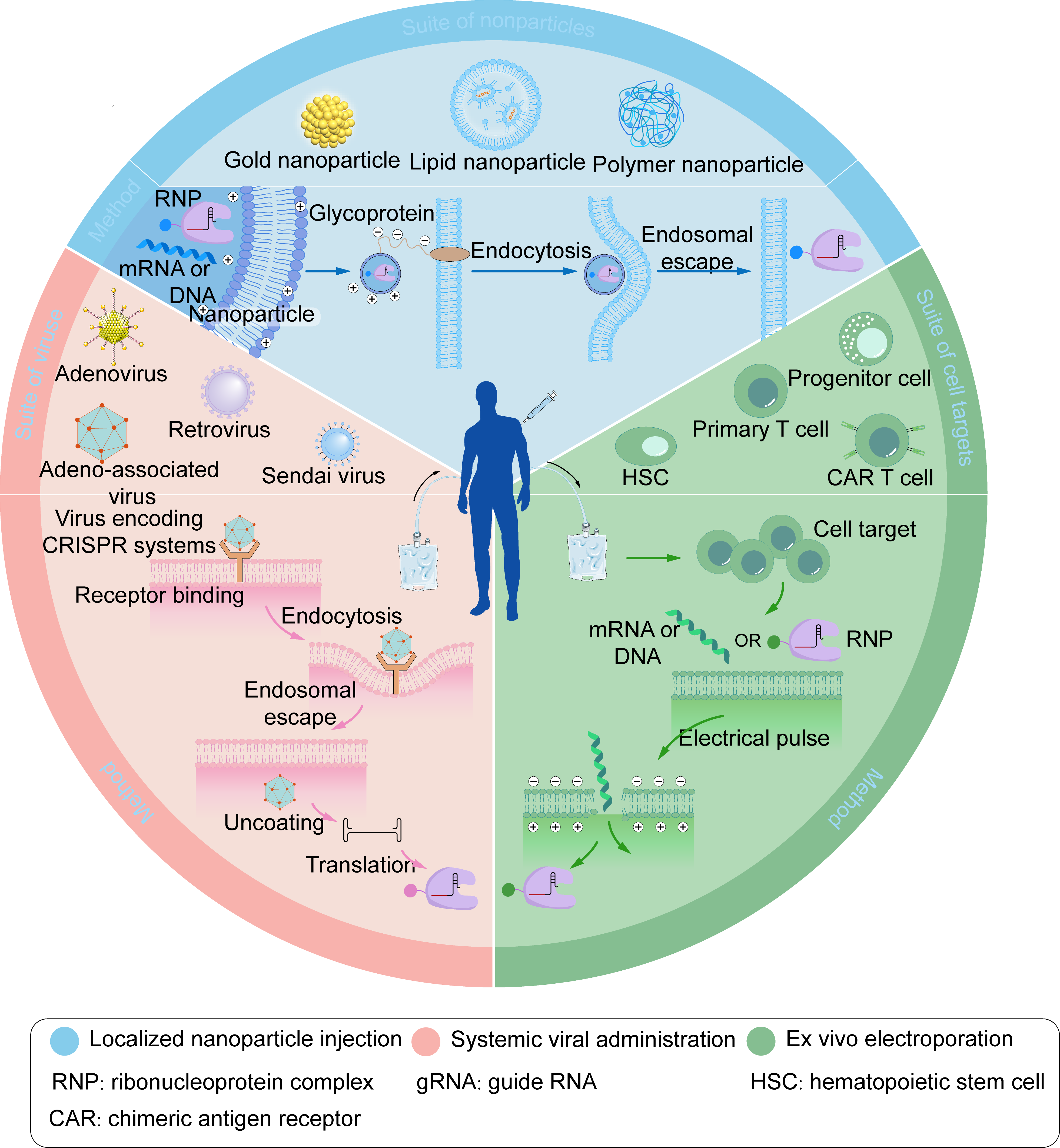
The tumor microenvironment (TME) can either promote or inhibit tumor initiation and progression, which may undergo changes at different stages of the disease. The CRISPR-Cas system, a revolutionary gene-editing tool, exhibits extensive potential in the analysis, diagnosis, and treatment of the tumor microenvironment, leveraging its ability to precisely target and edit specific genes. In this review, we first introduce the fundamental principles of CRISPR-Cas and discuss its applications in screening functional genes, dissecting cell-cell interactions, and analyzing dynamic changes within the tumor microenvironment. We then detail diagnosis platforms developed based on CRISPR-Cas system, which enable the sensitive detection across in vitro, organoid, and ex vivo settings. We also summarize different CRISPR-based cancer therapeutic strategies targeting the TME that enhance anti-tumor efficacy, including directly editing tumor cell, remodeling the immune microenvironment, as well as targeting the tumor vasculature and metabolic microenvironment. Additionally, the importance of delivery strategies is highlighted in this review. Finally, we summarize the existing challenges in this field, including off-target effects, immunogenicity, and the dynamic heterogeneity of the TME, while also exploring prospective research methodologies. This review aims to provide an overview of the field’s current state, offering insights for the development of new diagnostic and therapeutic strategies.
References
1. Hsu PD, Lander ES, Zhang F. Development and applications of CRISPR-Cas9 for genome engineering. Cell. 2014;157(6):1262-1278. doi:10.1016/j.cell.2014.05.010
2. Vink JNA, Baijens JHL, Brouns SJJ. PAM-repeat associations and spacer selection preferences in single and co-occurring CRISPR-Cas systems. Genome Biol. 2021;22(1):281. doi:10.1186/s13059-021-02495-9
3. Anzalone AV, Koblan LW, Liu DR. Genome editing with CRISPR-Cas nucleases, base editors, transposases and prime editors. Nat Biotechnol. 2020;38(7):824-844. doi:10.1038/s41587-020-0561-9
4. Deepak KGK, Vempati R, Nagaraju GP, Nagini S, Dasari VR, Rao DN, et al. Tumor microenvironment: challenges and opportunities in targeting metastasis of triple negative breast cancer. Pharmacol Res. 2020;153:104683. doi:10.1016/j.phrs.2020.104683
5. Tao J, Bauer DE, Chiarle R. Assessing and advancing the safety of CRISPR-Cas tools: from DNA to RNA editing. Nat Commun. 2023;14(1):212. doi:10.1038/s41467-023-35886-6
6. Yan WX, Hunnewell P, Alfonse LE, Carte J, Keston-Smith E, Sothiselvam S, et al. Functionally diverse type V CRISPR-Cas systems. Science. 2019;363(6422):88-91. doi:10.1126/science.aav7271
7. Jinek M, Chylinski K, Fonfara I, Hauer M, Doudna JA, Charpentier E. A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science. 2012;337(6096):816-821. doi:10.1126/science.1225829
8. Wang SW, Gao C, Zheng YM, Yi L, Lu JC, Huang XY, et al. Current applications and future perspective of CRISPR/Cas9 gene editing in cancer. Mol Cancer. 2022;21(1):57. doi:10.1186/s12943-022-01518-8
9. Deltcheva E, Chylinski K, Sharma CM, Gonzales K, Chao Y, Pirzada ZA, et al. CRISPR RNA maturation by trans-encoded small RNA and host factor RNase III. Nature. 2011;471(7340):602-607. doi:10.1038/nature09886
10. Doudna JA, Charpentier E. Genome editing. The new frontier of genome engineering with CRISPR-Cas9. Science.2014;346(6213):1258096. doi:10.1126/science.1258096
11. Sternberg SH, Redding S, Jinek M, Greene EC, Doudna JA. DNA interrogation by the CRISPR RNA-guided endonuclease Cas9. Nature. 2014;507(7490):62-67. doi:10.1038/nature13011
12. Bhatia S, Pooja, Yadav SK. CRISPR-Cas for genome editing: classification, mechanism, designing and applications. Int J Biol Macromol. 2023;238:124054. doi:10.1016/j.ijbiomac.2023.124054
13. Nishimasu H, Ran FA, Hsu PD, Konermann S, Shehata SI, Dohmae N, et al. Crystal structure of Cas9 in complex with guide RNA and target DNA. Cell. 2014;156(5):935-949. doi:10.1016/j.cell.2014.02.001
14. Sapranauskas R, Gasiunas G, Fremaux C, Barrangou R, Horvath P, Siksnys V. The streptococcus thermophilus CRISPR/Cas system provides immunity in Escherichia coli. Nucleic Acids Res. 2011;39(21):9275-9282. doi:10.1093/nar/gkr606
15. Xue C, Greene EC. DNA repair pathway choices in CRISPR-Cas9-mediated genome editing. Trends Genet. 2021;37(7):639-656. doi:10.1016/j.tig.2021.02.008
16. Bothmer A, Phadke T, Barrera LA, Margulies CM, Lee CS, Buquicchio F, et al. Characterization of the interplay between DNA repair and CRISPR/Cas9-induced DNA lesions at an endogenous locus. Nat Commun. 2017;8:13905. doi:10.1038/ncomms13905
17. Selvakumar SC, Preethi KA, Ross K, Tusubira D, Khan MWA, Mani P, et al. CRISPR/Cas9 and next generation sequencing in the personalized treatment of cancer. Mol Cancer. 2022;21(1):83. doi:10.1186/s12943-022-01565-1
18. Zetsche B, Gootenberg JS, Abudayyeh OO, Slaymaker IM, Makarova KS, Essletzbichler P, et al. Cpf1 is a single RNA-guided endonuclease of a class 2 CRISPR-Cas system. Cell. 2015;163(3):759-771. doi:10.1016/j.cell.2015.09.038
19. Shmakov S, Abudayyeh OO, Makarova KS, Wolf YI, Gootenberg JS, Semenova E, et al. Discovery and functional characterization of diverse class 2 CRISPR-Cas systems. Mol Cell. 2015;60(3):385-397. doi:10.1016/j.molcel.2015.10.008
20. Badon IW, Oh Y, Kim HJ, Lee SH. Recent application of CRISPR-Cas12 and OMEGA system for genome editing. Mol Ther. 2024;32(1):32-43. doi:10.1016/j.ymthe.2023.11.013
21. Yang H, Gao P, Rajashankar KR, Patel DJ. PAM-dependent target DNA recognition and cleavage by C2c1 CRISPR-Cas endonuclease. Cell. 2016;167(7):1814-1828.e12. doi:10.1016/j.cell.2016.11.053
22. Manghwar H, Lindsey K, Zhang X, Jin S. CRISPR/Cas system: recent advances and future prospects for genome editing. Trends Plant Sci. 2019;24(12):1102-1125. doi:10.1016/j.tplants.2019.09.006
23. Chen JS, Ma E, Harrington LB, Da Costa M, Tian X, Palefsky JM, et al. CRISPR-Cas12a target binding unleashes indiscriminate single-stranded DNase activity. Science. 2018;360(6387):436-439. doi:10.1126/science.aar6245
24. Li F, Li J, Yang W, Yang S, Chen C, Du L, et al. Framework-Hotspot Enhanced Trans Cleavage of CRISPR-Cas12a for Clinical Samples Detection. Angew Chem Int Ed Engl. 2023;62(32):e202305536. doi:10.1002/anie.202305536 doi:10.1002/anie.202305536
25.Wu S, Tian P, Tan T. CRISPR-Cas13 technology portfolio and alliance with other genetic tools. Biotechnol Adv. 2022;61:108047. doi:10.1016/j.biotechadv.2022.108047
26. Makarova KS, Wolf YI, Iranzo J, Shmakov SA, Alkhnbashi OS, Brouns SJJ, et al. Evolutionary classification of CRISPR-Cas systems: a burst of class 2 and derived variants. Nat Rev Microbiol. 2020;18(2):67-83. doi:10.1038/s41579-019-0299-x
27. Bot JF, van der Oost J, Geijsen N. The double life of CRISPR-Cas13. Curr Opin Biotechnol. 2022;78:102789. doi:10.1016/j.copbio.2022.102789
28. Dash PK, Chen C, Kaminski R, Su H, Mancuso P, Sillman B, et al. CRISPR editing of CCR5 and HIV-1 facilitates viral elimination in antiretroviral drug-suppressed virus-infected humanized mice. Proc Natl Acad Sci U S A. 2023;120(19):e2217887120. doi:10.1073/pnas.2217887120
29. Wu J, Xu H, Hu F, Jiang Y, Fan B, Khan A, et al. CRISPR-Cas and catalytic hairpin assembly technology for target-initiated amplification detection of pancreatic cancer specific tsRNAs. Front Bioeng Biotechnol. 2023;11:1169424. doi:10.3389/fbioe.2023.1169424
30. Wei Y, Fu Y, Li C, Chen S, Xie L, Chen M. Ultrasensitive detection of circulating tumor DNA using a CRISPR/Cas9 nickase-driven 3D DNA walker based on a COF-AuNPs sensing platform. Mikrochim Acta. 2024;191(11):671. doi:10.1007/s00604-024-06749-8
31. Wang Z, Li N, Feng K, Chen M, Zhang Y, Liu Y, et al. Phase I study of CAR-T cells with PD-1 and TCR disruption in mesothelin-positive solid tumors. Cell Mol Immunol. 2021;18(9):2188-2198. doi:10.1038/s41423-021-00749-x
32. Gootenberg JS, Abudayyeh OO, Lee JW, Essletzbichler P, Dy AJ, Joung J, et al. Nucleic acid detection with CRISPR-Cas13a/C2c2. Science. 2017;356(6336):438-442. doi:10.1126/science.aam9321
33. Wu X, Luo S, Guo C, Zhao Y, Zhong J, Hu R, et al. LbuCas13a directly targets DNA and elicits strong trans-cleavage activity. Nat Biomed Eng. 2025. doi:10.1038/s41551-025-01424-6
34. Hao L, Zhao RT, Welch NL, Tan EKW, Zhong Q, Harzallah NS, et al. CRISPR-Cas-amplified urinary biomarkers for multiplexed and portable cancer diagnostics. Nat Nanotechnol. 2023;18(7):798-807. doi:10.1038/s41565-023-01372-9
35. Ming M, Ren Q, Pan C, He Y, Zhang Y, Liu S, et al. CRISPR-Cas12b enables efficient plant genome engineering. Nat Plants. 2020;6(3):202-208. doi:10.1038/s41477-020-0614-6
36. Teng F, Cui T, Feng G, Guo L, Xu K, Gao Q, et al. Repurposing CRISPR-Cas12b for mammalian genome engineering. Cell Discov. 2018;4:63. doi:10.1038/s41421-018-0069-3
37. Teng F, Guo L, Cui T, Wang XG, Xu K, Gao Q, et al. CDetection: CRISPR-Cas12b-based DNA detection with sub-attomolar sensitivity and single-base specificity. Genome Biol. 2019;20(1):132. doi:10.1186/s13059-019-1742-z
38. Sam IK, Chen YY, Ma J, Li SY, Ying RY, Li LX, et al. TB-QUICK: CRISPR-Cas12b-assisted rapid and sensitive detection of Mycobacterium tuberculosis. J Infect. 2021;83(1):54-60. doi:10.1016/j.jinf.2021.04.032
39. Hu M, Liu R, Qiu Z, Cao F, Tian T, Lu Y, et al. Light-start CRISPR-Cas12a reaction with caged crRNAenables rapid and sensitive nucleic acid detection. Angew Chem Int Ed Engl. 2023;62(23):e202300663. doi:10.1002/anie.202300663
40. Chen Z, Arai E, Khan O, Zhang Z, Ngiow SF, He Y, et al. In vivo CD8+ T cell CRISPR screening reveals control by Fli1 in infection and cancer. Cell. 2021;184(5):1262-1280.e22. doi:10.1016/j.cell.2021.02.019
41. Chen J, Jiang Y, Hou M, Liu C, Liu E, Zong Y, et al. Nuclear translocation of plasma membrane protein ADCY7 potentiates T cell-mediated antitumour immunity in HCC. Gut. 2024;74(1):128-140. doi:10.1136/gutjnl-2024-332902
42. Wang C, Zheng X, Zhang J, Jiang X, Wang J, Li Y, et al. CD300ld on neutrophils is required for tumour-driven immune suppression. Nature. 2023;621(7980):830-839. doi:10.1038/s41586-023-06511-9
43. Wang X, Tokheim C, Gu SS, Wang B, Tang Q, Li Y, et al. In vivo CRISPR screens identify the E3 ligase Cop1 as a modulator of macrophage infiltration and cancer immunotherapy target. Cell. 2021;184(21):5357-5374.e22. doi:10.1016/j.cell.2021.09.006
44. Ye L, Park JJ, Peng L, Yang Q, Chow RD, Dong MB, et al. A genome-scale gain-of-function CRISPR screen in CD8 T cells identifies proline metabolism as a means to enhance CAR-T therapy. Cell Metab. 2022;34(4):595-614.e14. doi:10.1016/j.cmet.2022.02.009
45. Joung J, Kirchgatterer PC, Singh A, Cho JH, Nety SP, Larson RC, et al. CRISPR activation screen identifies BCL-2 proteins and B3GNT2 as drivers of cancer resistance to T cell-mediated cytotoxicity. Nat Commun. 2022;13(1):1606. doi:10.1038/s41467-022-29205-8
46. Li X, Sun S, Zhang W, Liang Z, Fang Y, Sun T, et al. Identification of genetic modifiers enhancing B7-H3-targeting CAR T cell therapy against glioblastoma through large-scale CRISPRi screening. J Exp Clin Cancer Res. 2024;43(1):95. doi:10.1186/s13046-024-03027-6
47. Zhu S, Cao Z, Liu Z, He Y, Wang Y, Yuan P, et al. Guide RNAs with embedded barcodes boost CRISPR-pooled screens. Genome Biol. 2019;20(1):20. doi:10.1186/s13059-019-1628-0
48. Hanna RE, Hegde M, Fagre CR, DeWeirdt PC, Sangree AK, Szegletes Z, et al. Massively parallel assessment of human variants with base editor screens. Cell. 2021;184(4):1064-1080.e20. doi:10.1016/j.cell.2021.01.012
49. Cuella-Martin R, Hayward SB, Fan X, Chen X, Huang JW, Taglialatela A, et al. Functional interrogation of DNA damage response variants with base editing screens. Cell. 2021;184(4):1081-1097.e19. doi:10.1016/j.cell.2021.01.041
50. Huang C, Li G, Wu J, Liang J, Wang X. Identification of pathogenic variants in cancer genes using base editing screens with editing efficiency correction. Genome Biol. 2021;22(1):80. doi:10.1186/s13059-021-02305-2
51. Xu P, Liu Z, Liu Y, Ma H, Xu Y, Bao Y, et al. Genome-wide interrogation of gene functions through base editor screens empowered by barcoded sgRNAs. Nat Biotechnol. 2021;39(11):1403-1413. doi:10.1038/s41587-021-00944-1
52. Coelho MA, Cooper S, Strauss ME, Karakoc E, Bhosle S, Gonçalves E, et al. Base editing screens map mutations affecting interferon-γ signaling in cancer. Cancer Cell. 2023;41(2):288-303.e6. doi:10.1016/j.ccell.2022.12.009
53. Schmidt R, Ward CC, Dajani R, Armour-Garb Z, Ota M, Allain V, et al. Base-editing mutagenesis maps alleles to tune human T cell functions. Nature. 2024;625(7996):805-812. doi:10.1038/s41586-023-06835-6
54. Adamson B, Norman TM, Jost M, Cho MY, Nunez JK, Chen Y, et al. A multiplexed single-cell CRISPR screening platform enables systematic dissection of the unfolded protein response. Cell. 2016;167(7):1867-1882.e21. doi:10.1016/j.cell.2016.11.048
55. Dixit A, Parnas O, Li B, Chen J, Fulco CP, Jerby-Arnon L, et al. Perturb-Seq: dissecting molecular circuits with scalable single-cell RNA profiling of pooled genetic screens. Cell. 2016;167(7):1853-1866.e17. doi:10.1016/j.cell.2016.11.038
56. Datlinger P, Rendeiro AF, Schmidl C, Krausgruber T, Traxler P, Klughammer J, et al. Pooled CRISPR screening with single-cell transcriptome readout. Nat Methods. 2017;14(3):297-301. doi:10.1038/nmeth.4177
57. Replogle JM, Norman TM, Xu A, Hussmann JA, Chen J, Cogan JZ, et al. Combinatorial single-cell CRISPR screens by direct guide RNA capture and targeted sequencing. Nat Biotechnol. 2020;38(8):954-961. doi:10.1038/s41587-020-0470-y
58. Fagerberg E, Attanasio J, Dien C, Singh J, Kessler EA, Abdullah L, et al. KLF2 maintains lineage fidelity and suppresses CD8 T cell exhaustion during acute LCMV infection. Science. 2025;387(6735):eadn2337. doi:10.1126/science.adn2337
59. Renz PF, Ghoshdastider U, Baghai Sain S, Valdivia-Francia F, Khandekar A, Ormiston M, et al. In vivo single-cell CRISPR uncovers distinct TNF programmes in tumour evolution. Nature. 2024;632(8024):419-428. doi:10.1038/s41586-024-07663-y
60. DeWeirdt PC, Sanson KR, Sangree AK, Hegde M, Hanna RE, Feeley MN, et al. Optimization of AsCas12a for combinatorial genetic screens in human cells. Nat Biotechnol. 2021;39(1):94-104. doi:10.1038/s41587-020-0600-6
61. Konermann S, Lotfy P, Brideau NJ, Oki J, Shokhirev MN, Hsu PD. Transcriptome engineering with RNA-targeting type VI-D CRISPR effectors. Cell. 2018;173(3):665-676.e14. doi:10.1016/j.cell.2018.02.033
62. Abudayyeh OO, Gootenberg JS, Essletzbichler P, Han S, Joung J, Belanto JJ, et al. RNA targeting with CRISPR-Cas13. Nature. 2017;550(7675):280-284. doi:10.1038/nature24049
63. Li S, Li X, Xue W, Zhang L, Yang LZ, Cao SM, et al. Screening for functional circular RNAs using the CRISPR-Cas13 system. Nat Methods. 2021;18(1):51-59. doi:10.1038/s41592-020-01011-4
64. Si J, Su X, Jin Z, Duan S. Uncovering essential lncRNAs through transcriptome-scale CRISPR-Cas13 screening. Adv Biotechnol (Singap). 2025;3(3):27. doi:10.1007/s44307-025-00082-8
65. Zhou P, Shi H, Huang H, Sun X, Yuan S, Chapman NM, et al. Single-cell CRISPR screens in vivo map T cell fate regulomes in cancer. Nature;624(7990):154-163. doi:10.1038/s41586-023-06733-x
66. Dubrot J, Du PP, Lane-Reticker SK, Kessler EA, Muscato AJ, Mehta A, et al. In vivo CRISPR screens reveal the landscape of immune evasion pathways across cancer. Nat Immunol. 2022;23(10):1495-1506. doi:10.1038/s41590-022-01315-x
67. Burr ML, Sparbier CE, Chan KL, Chan YC, Kersbergen A, Lam EYN, et la. An evolutionarily conserved function of Polycomb silences the MHC class I antigen presentation pathway and enables immune evasion in cancer. Cancer Cell. 2019;36(4):385-401.e8. doi:10.1016/j.ccell.2019.08.008
68. Chen X, Lu Q, Zhou H, Liu J, Nadorp B, Lasry A, et al. A membrane-associated MHC-I inhibitory axis for cancer immune evasion. Cell. 2023;186(18):3903-3920.e21. doi:10.1016/j.cell.2023.07.016
69. Fu L, Li S, Mei J, Li Z, Yang X, Zheng C, et al. BIRC2 blockade facilitates immunotherapy of hepatocellular carcinoma. Mol Cancer. 2025;24(1):113. doi:10.1186/s12943-02502319-5
70. Binan L, Jiang A, Danquah SA, Valakh V, Simonton B, Bezney J, et al. Simultaneous CRISPR screening and spatial transcriptomics reveal intracellular, intercellular, and functional transcriptional circuits. Cell. 2025;188(8):2141-2158.e18. doi:10.1016/j.cell.2025.02.012
71. Rogers ZN, McFarland CD, Winters IP, Seoane JA, Brady JJ, Yoon S, et al. Mapping the in vivo fitness landscape of lung adenocarcinoma tumor suppression in mice. Nat Genet. 2018;50(4):483-486. doi:10.1038/s41588-018-0083-2
72. Bowling S, Sritharan D, Osorio FG, Nguyen M, Cheung P, Rodriguez-Fraticelli A, et al. An engineered CRISPR-Cas9 mouse line for simultaneous readout of lineage histories and gene expression profiles in single cells. Cell. 2020;181(6):1410-1422.e27. doi:10.1016/j.cell.2020.04.048
73. Li L, Bowling S, McGeary SE, Yu Q, Lemke B, Alcedo K, et al. A mouse model with high clonal barcode diversity for joint lineage, transcriptomic, and epigenomic profiling in single cells. Cell. 2023;186(23):5183-5199.e22. doi:10.1016/j.cell.2023.09.019
74. Xie L, Liu H, You Z, Wang L, Li Y, Zhang X, et al. Comprehensive spatiotemporal mapping of single-cell lineages in developing mouse brain by CRISPR-based barcoding. Nat Methods. 2023;20(8):1244-1255. doi:10.1038/s41592-023-01947-3
75. Chan MM, Smith ZD, Grosswendt S, Kretzmer H, Norman TM, Adamson B, et al. Molecular recording of mammalian embryogenesis. Nature. 2019;570(7759):77-82. doi:10.1038/s41586-019-1184-5
76. Quinn JJ, Jones MG, Okimoto RA, Nanjo S, Chan MM, Yosef N, et al. Single-cell lineages reveal the rates, routes, and drivers of metastasis in cancer xenografts. Science. 2021;371(6532):eabc1944. doi:10.1126/science.abc1944
77. Wang S, Shen X, Chen G, Zhang W, Tan B. Application and development of CRISPR-Cas12a methods for the molecular diagnosis of cancer: a review. Anal Chim Acta. 2025;1341:343603. doi:10.1016/j.aca.2024.343603
78. Chen M, Wu D, Tu S, Yang C, Chen D, Xu Y. CRISPR/Cas9 cleavage triggered ESDR for circulating tumor DNA detection based on a 3D graphene/AuPtPd nanoflower biosensor. Biosens Bioelectron. 2021;173:112821. doi:10.1016/j.bios.2020.112821
79. Sahel DK, Giriprasad G, Jatyan R, Guha S, Korde A, Mittal A, et al. Next-generation CRISPR/Cas-based ultrasensitive diagnostic tools: current progress and prospects. RSC Adv. 2024;14(44):32411-32435. doi:10.1039/d4ra04838e
80. Dong JL, Xu Z, Zhang L, Chen M, Yu J, Zhou H, et al. Comparative evaluation of PCR-based, LAMP and RPA-CRISPR/Cas12a assays for the rapid detection of Diaporthe aspalathi. Int J Mol Sci. 2024;25(11):15773. doi:10.3390/ijms25115773
81. Gu W, Crawford ED, O'Donovan BD, Wilson MR, Chow ED, Retallack H, et al. Depletion of abundant sequences by hybridization (DASH): using Cas9 to remove unwanted high-abundance species in sequencing libraries and molecular counting applications. Genome Biol. 2016;17:41. doi:10.1186/s13059-016-0904-5
82. Kleinstiver BP, Prew MS, Tsai SQ, Topkar VV, Nguyen NT, Zheng Z, et al. Engineered CRISPR-Cas9 nucleases with altered PAM specificities. Nature. 2015;523(7561):481-485. doi:10.1038/nature14592
83. Li SY, Cheng QX, Liu JK, Nie XQ, Zhao GP, Wang J. CRISPR-Cas12a has both cis- and trans-cleavage activities on single-stranded DNA. Cell Res. 2018;28(4):491-493. doi:10.1038/s41422-018-0022-x
84. Chen J, Chen Y, Huang L, Lin X, Chen H, Xiang W, et al. Trans-nuclease activity of Cas9 activated by DNA or RNA target binding. Nat Biotechnol. 2025;43(4):558-568. doi:10.1038/s41587-024-02255-7
85. Nguyen LT, Smith BM, Jain PK. Enhancement of trans-cleavage activity of Cas12a with engineered crRNA enables amplified nucleic acid detection. Nat Commun. 2020;11(1):4906. doi:10.1038/s41467-020-18615-1
86. Yan H, Wen Y, Tian Z, Hart N, Han S, Hughes SJ, et al. A one-pot isothermal Cas12-based assay for the sensitive detection of microRNAs. Nat Biomed Eng. 2023;7(12):1583-1601. doi:10.1038/s41551-023-01033-1
87. Yan H, Wen Y, Tian Z, Hart N, Han S, Hughes SJ, Zeng Y. A one-pot isothermal Cas12-based assay for the sensitive detection of microRNAs. Nat Biomed Eng. 2023;7(12):1583-1601. doi:10.1038/s41551-023-01033-1
88. Rananaware SR, Vesco EK, Shoemaker GM, Anekar SS, Sandoval LSW, Meister KS, et al. Programmable RNA detection with CRISPR-Cas12a. Nat Commun. 2023;14(1):5409. doi:10.1038/s41467-023-41006-1
89. Chen Y, Wang X, Zhang J, Jiang Q, Qiao B, He B, et la. Split crRNA with CRISPR-Cas12a enabling highly sensitive and multiplexed detection of RNA and DNA. Nat Commun. 2024;15(1):8342. doi:10.1038/s41467-024-52691-x
90. Moon J, Liu C. Asymmetric CRISPR enabling cascade signal amplification for nucleic acid detection by competitive crRNA. Nat Commun. 2023;14(1):7504. doi:10.1038/s41467-023-43389-7
91. van Dongen JE, Berendsen JTW, Eijkel JCT, Segerink LI. A CRISPR/Cas12a-assisted in vitro diagnostic tool for identification and quantification of single CpG methylation sites. Biosens Bioelectron. 2021;194:113624. doi:10.1016/j.bios.2021.113624
92. Krysler AR, Cromwell CR, Tu T, Jovel J, Hubbard BP. Guide RNAs containing universal bases enable Cas9/Cas12a recognition of polymorphic sequences. Nat Commun. 2022;13(1):1617. doi:10.1038/s41467-022-29202-x
93. Kocak DD, Josephs EA, Bhandarkar V, Adkar SS, Kwon JB, Gersbach CA. Increasing the specificity of CRISPR systems with engineered RNA secondary structures. Nat Biotechnol. 2019;37(6):657-666. doi:10.1038/s41587-019-0095-1
94. Yin H, Song CQ, Suresh S, Kwan SY, Wu Q, Walsh S, et al. Partial DNA-guided Cas9 enables genome editing with reduced off-target activity. Nat Chem Biol. 2018;14(3):311-316. doi:10.1038/nchembio.2559
95. Kleinstiver BP, Pattanayak V, Prew MS, Tsai SQ, Nguyen NT, Zheng Z, et al. High-fidelity CRISPR-Cas9 nucleases with no detectable genome-wide off-target effects. Nature. 2016;529(7587):490-495. doi:10.1038/nature16526
96. Chen L, Hu M, Zhou X. Trends in developing one-pot CRISPR diagnostics strategies. Trends Biotechnol. 2025;43(1):98-110. doi:10.1016/j.tibtech.2024.07.007
97. Huang W, Wang J, Wang C, Liu Y, Li W, Chen Q, et al. Expanding Cas12a activity control with an RNA G-quadruplex at the 5' end of CRISPR RNA. Adv Sci (Weinh). 2025;12(7):e2411305. doi:10.1002/advs.202411305
98. Zhang W, Zhong Y, Wang J, Zou G, Chen Q, Liu C. Direct repeat region 3' end modifications regulate Cas12a activity and expand its applications. Nucleic Acids Res. 2025;53(3):gkaf040doi:10.1093/nar/gkaf040
99. Lin M, Qiu Z, Hao M, Qi W, Zhang T, Shen Y, et al. Cas12a cis-cleavage mediated lateral flow assay enables multiplex and ultra-specific nucleic acid detection. Nat Commun. 2025;16(1):5597. doi:10.1038/s41467-025-60917-9
100. Labib M, Kelley SO. Single-cell analysis targeting the proteome. Nat Rev Chem. 2020;4(3):143-158. doi:10.1038/s41570-020-0162-7
101. Jaitin DA, Weiner A, Yofe I, Lara-Astiaso D, Keren-Shaul H, David E, et al. Dissecting immune circuits by linking CRISPR-pooled screens with single-cell RNA-seq. Cell. 2016;167(7):1883-1896.e15. doi:10.1016/j.cell.2016.11.039
102. Li Y, Huang Z, Xu L, Fan Y, Ping J, Li G, et al. UDA-seq: universal droplet microfluidics-based combinatorial indexing for massive-scale multimodal single-cell sequencing. Nat Methods. 2025;22(6):1199-1212. doi:10.1038/s41592-024-02586-y
103. Metzner E, Southard KM, Norman TM. Multiome perturb-seq unlocks scalable discovery of integrated perturbation effects on the transcriptome and epigenome. Cell Syst. 2025;16(1):101161. doi:10.1016/j.cels.2024.12.002
104. Schraivogel D, Gschwind AR, Milbank JH, Leonce DR, Jakob P, Mathur L, et al. Targeted Perturb-seq enables genome-scale genetic screens in single cells. Nat Methods. 2020;17(6):629-635. doi:10.1038/s41592-020-0837-5
105. Yao D, Binan L, Bezney J, Simonton B, Freedman J, Frangieh CJ, et al. Scalable genetic screening for regulatory circuits using compressed Perturb-seq. Nat Biotechnol. 2024;42(8):1282-1295. doi:10.1038/s41587-023-01964-9
106. Wroblewska A, Dhainaut M, Ben-Zvi B, Rose SA, Park ES, Amir ED, et al. Protein barcodes enable high-dimensional single-cell CRISPR screens. Cell. 2018;175(4):1141-1155.e16. doi:10.1016/j.cell.2018.09.022
107. Dhainaut M, Rose SA, Akturk G, Wroblewska A, Nielsen SR, Park ES, et al. Spatial CRISPR genomics identifies regulators of the tumor microenvironment. Cell. 2022;185(7):1223-1239.e20. doi:10.1016/j.cell.2022.02.015
108. Tang L. Spatial CRISPR screens in tumors. Nat Methods. 2022;19(5):517. doi:10.1038/s41592-022-01501-7
109. Park YM, Lin D-C. Moving closer towards a comprehensive view of tumor biology and microarchitecture using spatial transcriptomics. Nat Commun. 2023;14(1):7017. doi:10.1038/s41467-023-42960-6
110. Rausch M, Bartels K, Leibold J. Immunotherapy in ovarian cancer: spatial functional genomics to unravel resistance mechanisms. Signal Transduct Target Ther. 2025;10(1):17. doi:10.1038/s41392-024-02110-w
111. Binan L. Investigating spatial gene circuits and gene-phenotype mechanisms with Perturb-FISH. Nat Rev Genet. 2025;26(8):507-508. doi:10.1038/s41576-025-00857-8
112. Kudo T, Meireles AM, Moncada R, Chen Y, Wu P, Gould J, et al. Multiplexed, image-based pooled screens in primary cells and tissues with PerturbView. Nat Biotechnol. 2025;43(7):1091-1100. doi:10.1038/s41587-024-02391-0
113. Hu Y, An Q, Sheu K, Trejo B, Fan S, Guo Y. Single cell multi-omics technology: methodology and application. Front Cell Dev Biol. 2018;6:28. doi:10.3389/fcell.2018.00028
114. Frangieh CJ, Melms JC, Thakore PI, Geiger-Schuller K, Ho P, Luoma AM, et al. Multimodal pooled perturb-CITE-seq screens in patient models define mechanisms of cancer immune evasion. Nat Genet. 2021;53(3):332-341. doi:10.1038/s41588-021-00779-1
115. Vandereyken K, Sifrim A, Thienpont B, Voet T. Methods and applications for single-cell and spatial multi-omics. Nat Rev Genet. 2023;24(8):494-515. doi:10.1038/s41576-023-00580-2
116. Minnoye L, Marinov GK, Krausgruber T, Pan L, Marand AP, Secchia S, et al. Chromatin accessibility profiling methods. Nat Rev Methods Primers. 2021;1:10. doi:10.1038/s43586-020-00008-9
117. Grandi FC, Modi H, Kampman L, Corces MR. Chromatin accessibility profiling by ATAC-seq. Nat Protoc. 2022;17(6):1518-1552. doi:10.1038/s41596-022-00692-9
118. Pierce SE, Granja JM, Greenleaf WJ. High-throughput single-cell chromatin accessibility CRISPR screens enable unbiased identification of regulatory networks in cancer. Nat Commun. 2021;12(1):2969. doi:10.1038/s41467-021-23213-w
119. Liscovitch-Brauer N, Montalbano A, Deng J, Méndez-Mancilla A, Wessels H-H, Moss NG, et al. Profiling the genetic determinants of chromatin accessibility with scalable single-cell CRISPR screens. Nat Biotechnol. 2021;39(10):1270-1277. doi:10.1038/s41587-021-00902-x
120. Replogle JM, Saunders RA, Pogson AN, Hussmann JA, Lenail A, Guna A, et al. Mapping information-rich genotype-phenotype landscapes with genome-scale Perturb-seq. Cell. 2022;185(14):2559-2575.e28. doi:10.1016/j.cell.2022.05.013
121. Szlachta K, Kuscu C, Tufan T, Adair SJ, Shang S, Michaels AD, et al. CRISPR knockout screening identifies combinatorial drug targets in pancreatic cancer and models cellular drug response. Nat Commun. 2018;9(1):4275. doi:10.1038/s41467-018-06676-2
122. Qu J, Kalyani FS, Liu L, Cheng T, Chen L. Tumor organoids: synergistic applications, current challenges, and future prospects in cancer therapy. Cancer Commun (Lond). 2021;41(12):1331-1353. doi:10.1002/cac2.12224
123. Lo YH, Horn HT, Huang MF, Yu WC, Young CM, Liu Q, et al. Large-scale CRISPR screening in primary human 3D gastric organoids enables comprehensive dissection of gene-drug interactions. Nat Commun. 2025;16(1):7566. doi:10.1038/s41467-025-62818-3
124. Shi H, Doench JG, Chi H. CRISPR screens for functional interrogation of immunity. Nat Rev Immunol. 2023;23(6):363-380. doi:10.1038/s41577-022-00802-4
125. Oldrini B, Curiel García Á, Marques C, Matia V, Uluçkan O, Graña-Castro O, et al. Somatic genome editing with the RCAS-TVA-CRISPR-Cas9 system for precision tumor modeling. Nat Commun. 2018;9(1):1466. doi:10.1038/s41467-018-03731-w
126. Su P, Liu Y, Chen T, Xue Y, Zeng Y, Zhu G, et al. In vivo CRISPR screens identify a dual function of MEN1 in regulating tumor-microenvironment interactions. Nat Genet. 2024;56(9):1890-1902. doi:10.1038/s41588-024-01874-9
127. Dervovic D, Malik AA, Chen ELY, Narimatsu M, Adler N, Afiuni-Zadeh S, et al. In vivo CRISPR screens reveal Serpinb9 and Adam2 as regulators of immune therapy response in lung cancer. Nat Commun. 2023;14(1):3150. doi:10.1038/s41467-023-38841-7
128. Wei J, Long L, Zheng W, Dhungana Y, Lim SA, Guy C, et al. Targeting REGNASE-1 programs long-lived effector T cells for cancer therapy. Nature. 2019;576(7787):471-476. doi:10.1038/s41586-019-1821-z
129. Dong MB, Wang G, Chow RD, Ye L, Zhu L, Dai X, et al. Systematic immunotherapy target discovery using genome-scale in vivo CRISPR screens in CD8 T cells. Cell. 2019;178(5):1189-1204.e23. doi:10.1016/j.cell.2019.07.044
130. Ye L, Park JJ, Dong MB, Yang Q, Chow RD, Peng L, et al. In vivo CRISPR screening in CD8 T cells with AAV-Sleeping Beauty hybrid vectors identifies membrane targets for improving immunotherapy for glioblastoma. Nat Biotechnol. 2019;37(11):1302-1313. doi:10.1038/s41587-019-0246-4
131. Mimitou EP, Cheng A, Montalbano A, Hao S, Stoeckius M, Legut M, et al. Multiplexed detection of proteins, transcriptomes, clonotypes and CRISPR perturbations in single cells. Nat Methods. 2019;16(5):409-412. doi:10.1038/s41592-019-0392-0
132. Tang L. Tackling in vivo screening complexity. Nat Methods. 2025;22(2):224. doi:10.1038/s41592-025-02605-6
133. Uijttewaal ECH, Lee J, Sell AC, Botay N, Vainorius G, Novatchkova M, et al. CRISPR-StAR enables high-resolution genetic screening in complex in vivo models. Nat Biotechnol. 2025;43(11):1848-1860. doi:10.1038/s41587-024-02512-9
134. Lu M, Shao W, Xing H, Huang Y. Extracellular vesicle-based nucleic acid delivery. Interdiscip Med. 2023;1:100007. doi:10.1002/inmd.20220007
135. Xu X, Liu C, Wang Y, Koivisto O, Zhou J, Shu Y, et al. Nanotechnology-based delivery of CRISPR/Cas9 for cancer treatment. Adv Drug Deliv Rev. 2021;176:113891. doi:10.1016/j.addr.2021.113891
136. Glass Z, Lee M, Li Y, Xu Q. Engineering the delivery system for CRISPR-based genome editing. Trends Biotechnol. 2018;36(2):173-185. doi:10.1016/j.tibtech.2017.11.006
137. Porto EM, Komor AC, Slaymaker IM, Yeo GW. Base editing: advances and therapeutic opportunities. Nat Rev Drug Discov. 2020;19(12):839-859. doi:10.1038/s41573-020-0084-6
138. Madigan V, Zhang F, Dahlman JE. Drug delivery systems for CRISPR-based genome editors. Nat Rev Drug Discov. 2023;22(11):875-894. doi:10.1038/s41573-023-00762-x
139. Song X, Liu C, Wang N, Huang H, He S, Gong C, et al. Delivery of CRISPR/Cas systems for cancer gene therapy and immunotherapy. Adv Drug Deliv Rev. 2021;168:158-180. doi:10.1016/j.addr.2020.04.010
140. Wang X, Wei M, Miao R, Hao X, Li M, Wang W, et al. Adeno-associated virus vectors for gene therapy—focusing on melanoma. Interdiscip Med. 2024;2(4):100031. doi:10.1002/inmd.20240031
141. Wang D, Tai PWL, Gao G. Adeno-associated virus vector as a platform for gene therapy delivery. Nat Rev Drug Discov. 2019;18(5):358-378. doi:10.1038/s41573-019-0012-9
142. Ran FA, Cong L, Yan WX, Scott DA, Gootenberg JS, Kriz AJ, et al. In vivo genome editing using Staphylococcus aureus Cas9. Nature. 2015;520(7546):186-191. doi:10.1038/nature14299
143. Esvelt KM, Mali P, Braff JL, Moosburner M, Yaung SJ, Church GM. Orthogonal Cas9 proteins for RNA-guided gene regulation and editing. Nat Methods. 2013;10(11):1116-1121. doi:10.1038/nmeth.2681
144. Hou Z, Zhang Y, Propson NE, Howden SE, Chu L-F, Sontheimer EJ, et al. Efficient genome engineering in human pluripotent stem cells using Cas9 from Neisseria meningitidis. Proc Natl Acad Sci U S A. 2013;110(39):15644-15649. doi:10.1073/pnas.1313587110
145. Kim E, Koo T, Park SW, Kim D, Kim K, Cho H-Y, et al. In vivo genome editing with a small Cas9 orthologue derived from Campylobacter jejuni. Nat Commun. 2017;8:14500. doi:10.1038/ncomms14500
146. Hu Z, Zhang C, Wang S, Gao S, Wei J, Li M, et al. Discovery and engineering of small SlugCas9 with broad targeting range and high specificity and activity. Nucleic Acids Res. 2021;49(7):4008-4019. doi:10.1093/nar/gkab148
147. Edraki A, Mir A, Ibraheim R, Gainetdinov I, Yoon Y, Song C-Q, et al. A compact, high-accuracy Cas9 with a dinucleotide PAM for in vivo genome editing. Mol Cell. 2019;73(4):714-726.e4. doi:10.1016/j.molcel.2018.12.003
148. Schuler G, Hu C, Ke A. Structural basis for RNA-guided DNA cleavage by IscB-ωRNA and mechanistic comparison with Cas9. Science. 2022;376(6600):1476-1481. doi:10.1126/science.abq7220
149. Teng F, Cui T, Gao Q, Guo L, Zhou Q, Li W. Artificial sgRNAs engineered for genome editing with new Cas12b orthologs. Cell Discov. 2019;5:23. doi:10.1038/s41421-019-0091-0
150. Strecker J, Jones S, Koopal B, Schmid-Burgk J, Zetsche B, Gao L, et al. Engineering of CRISPR-Cas12b for human genome editing. Nat Commun. 2019;10(1):212. doi:10.1038/s41467-018-08224-4
151. Liu JJ, Orlova N, Oakes BL, Ma E, Spinner HB, Baney KLM, et al. Casx enzymes comprise a distinct family of RNA-guided genome editors. Nature. 2019;566(7743):218-223. doi:10.1038/s41586-019-0908-x
152. Pausch P, Al-Shayeb B, Bisom-Rapp E, Tsuchida CA, Li Z, Cress BF, et al. CRISPR-CasΦ from huge phages is a hypercompact genome editor. Science. 2020;369(6501):333-337. doi:10.1126/science.abb1400
153. Kim DY, Lee JM, Moon SB, Chin HJ, Park S, Lim Y, et al. Efficient CRISPR editing with a hypercompact Cas12f1 and engineered guide RNAs delivered by adeno-associated virus. Nat Biotechnol. 2022;40(1):94-102. doi:10.1038/s41587-021-01009-z
154. Chen L, Zhou X, Huang C, Zhang Y, Xin C, Hong J, et al. Engineered Un1Cas12f1 with boosted gene-editing activity and expanded genomic coverage. Proc Natl Acad Sci U S A. 2025;122(32):e2501292122. doi:10.1073/pnas.2501292122
155. Ma S, Liao K, Chen K, Cheng T, Yang X, Chen P, et al. hpCasMINI: An engineered hypercompact CRISPR-Cas12f system with boosted gene editing activity. Nat Commun. 2025;16(1):5001. doi:10.1038/s41467-025-60124-6
156. Liao K, Chen K, Ma S, Yang X, Chen P, Li S, et al. exoCasMINI: A T5 exonuclease fused CRISPR-Cas12f system with enhanced gene editing efficiency. iScience. 2025;28(8):113171. doi:10.1016/j.isci.2025.113171
157. Kannan S, Altae-Tran H, Jin X, Madigan VJ, Oshiro R, Makarova KS, et al. Compact RNA editors with small Cas13 proteins. Nat Biotechnol. 2022;40(2):194-197. doi:10.1038/s41587-021-01030-2
158. Xu C, Zhou Y, Xiao Q, He B, Geng G, Wang Z, et al. Programmable RNA editing with compact CRISPR-Cas13 systems from uncultivated microbes. Nat Methods. 2021;18(5):499-506. doi:10.1038/s41592-021-01124-4
159. Yu C, Li L, Hu P, Yang Y, Wei W, Deng X, et al. Recent advances in stimulus-responsive nanocarriers for gene therapy. Adv Sci (Weinh). 2021;8(14):2100540. doi:10.1002/advs.202100540
160. Tang N, Ning Q, Wang Z, Tao Y, Zhao X, Tang S. Tumor microenvironment based stimuli-responsive CRISPR/Cas delivery systems: A viable platform for interventional approaches. Colloids Surf B Biointerfaces. 2022;210:112257. doi:10.1016/j.colsurfb.2021.112257
161. Xing Y, Yang J, Wang Y, Wang C, Pan Z, Liu FL, et al. Remodeling tumor immunogenicity with dual-activatable binary CRISPR nanomedicine for cancer immunotherapy. ACS Nano. 2023;17(6):5713-5726. doi:10.1021/acsnano.2c12107
162. Costagliola di Polidoro A, Cafarchio A, Vecchione D, Donato P, De Nola F, Torino E. Revealing Angiopep-2/LRP1 molecular interaction for optimal delivery to glioblastoma (GBM). Molecules. 2022;27(19):6696. doi:10.3390/molecules27196696
163. Zhao Y, Qin J, Yu D, Liu Y, Song D, Tian K. Polymer-locking fusogenic liposomes for glioblastoma-targeted siRNA delivery and CRISPR-Cas gene editing. Nat Nanotechnol. 2024;19(12):1869-1879. doi:10.1038/s41565-024-01769-0
164. Zou C, Liu X, Wang W, He L, Yin A, Cao Z, et al. Targeting GDF15 to enhance immunotherapy efficacy in glioblastoma through tumor microenvironment-responsive CRISPR-Cas9 nanoparticles. J Nanobiotechnology. 2025;23(1):126. doi:10.1186/s12951-025-03182-8
165. Zhao K, Yan Y, Jin XK, Pan T, Zhang SM, Yang CH, et al. An orally administered gene editing nanoparticle boosts chemo-immunotherapy in colorectal cancer. Nat Nanotechnol. 2025;20(7):935-946. doi:10.1038/s41565-025-01904-5
166. Zhao W, Zhang L, Guo J, Xu Q, Zhang M, Liu H, et al. Intelligent nano-cage for precision delivery of CRISPR-Cas9 and ACC inhibitors to enhance antitumor cascade therapy through lipid metabolism disruption. Adv Funct Mater. 2025;35(13)2418090. doi:10.1002/adfm.202418090
167. Liu H, Yang Y, Zhang N, Hou Y, Zhang Z, Yu X, et al. Overcoming photothermal resistance of gastric cancer by bionic 2D iron-based nanoplatforms with precise CRISPR/Cas9 delivery. ACS Nano. ACS Nano. 2025;19(19):18188-18202. doi:10.1021/acsnano.4c16846
168. Awwad SW, Serrano-Benitez A, Thomas JC, Gupta V, Jackson SP. Revolutionizing DNA repair research and cancer therapy with CRISPR-Cas screens. Nat Rev Mol Cell Biol. 2023;24(7):477-494. doi:10.1038/s41580-022-00571-x
169. Zhang A, Miao K, Sun H, Deng CX. Tumor heterogeneity reshapes the tumor microenvironment to influence drug resistance. Int J Biol Sci. 2022;18(7):3019-3033. doi:10.7150/ijbs.72534
170. Azangou-Khyavy M, Ghasemi M, Khanali J, Boroomand-Saboor M, Jamalkhah M, Soleimani M, et la. CRISPR/Cas: From tumor gene editing to T cell-based immunotherapy of cancer. Front Immunol. 2020;11:2062. doi:10.3389/fimmu.2020.02062
171. Chehelgerdi M, Chehelgerdi M, Khorramian-Ghahfarokhi M, Shafieizadeh M, Mahmoudi E, Eskandari F, et al. Comprehensive review of CRISPR-based gene editing: mechanisms, challenges, and applications in cancer therapy. Mol Cancer. 2024;23(1):9. doi:10.1186/s12943-023-01925-5
172. Di Carlo E, Sorrentino C. State of the art CRISPR-based strategies for cancer diagnostics and treatment. Biomark Res. 2024;12(1):156. doi:10.1186/s40364-024-00701-x
173. Martinez-Lage M, Torres-Ruiz R, Puig-Serra P, Moreno-Gaona P, Martin MC, Moya FJ, et al. In vivo CRISPR/Cas9 targeting of fusion oncogenes for selective elimination of cancer cells. Nat Commun. 2020;11(1):5060. doi:10.1038/s41467-020-18875-x
174. Duan Y, Liu Z, Wang Q, Zhang J, Liu J, Zhang Z, et al. Targeting MYC: Multidimensional regulation and therapeutic strategies in oncology. Genes Dis. 2024;12(4):101435. doi:10.1016/j.gendis.2024.101435
175. Kim W, Lee S, Kim HS, Song M, Cha YH, Kim YH, et al. Targeting mutant KRAS with CRISPR-Cas9 controls tumor growth. Genome Res. 2018;28:374-382. doi:10.1101/gr.223891.117
176. Wei Y, Zhao Z, Ma X. Description of CRISPR-Cas9 development and its prospects in human papillomavirus-driven cancer treatment. Front Immunol. 2022;13:1037124. doi:10.3389/fimmu.2022.1037124
177. Jin X, Lou X, Qi H, Zheng C, Li B, Siwu X, et al. NRF2 signaling plays an essential role in cancer progression through the NRF2-GPX2-NOTCH3 axis in head and neck squamous cell carcinoma. Oncogenesis. 2024;13:35. doi:10.1038/s41389-024-00536-z
178. Hussen BM, Najmadden ZB, Abdullah SR, Rasul MF, Mustafa SA, Ghafouri-Fard et al. CRISPR/Cas9 gene editing: a novel strategy for fighting drug resistance in respiratory disorders. Cell Commun Signal. 2024;22:329. doi:10.1186/s12964-024-01713-8
179. Chen Y, Zhang Y. Application of the CRISPR/Cas9 system to drug resistance in breast cancer. Adv Sci (Weinh). 2018;5:1700964. doi:10.1002/advs.201700964
180. Di Cristofano A, Pandolfi PP. The multiple roles of PTEN in tumor suppression. Cell. 2000;100(4):387-390. doi:10.1016/s0092-8674(00)80674-1
181. Vitiello M, Evangelista M, Zhang Y, Salmena L, Pandolfi PP, Poliseno L. PTENP1 is a ceRNA for PTEN: it’s CRISPR clear. J Hematol Oncol. 2020;13:73. doi:10.1186/s13045-020-00894-2
182. Tang W, Liu J, Ding B. Nucleic acid nanostructure for delivery of CRISPR/Cas9-based gene editing system. Interdiscip Med. 2023;1:e20220014. doi:10.1002/inmd.20220014
183. Guo LY, Bian J, Davis AE, Liu P, Kempton HR, Zhang X, et al. Multiplexed genome regulation in vivo with hyper-efficient Cas12a. Nat Cell Biol. 2022;24:590-600. doi:10.1038/s41556-022-00870-7
184. Li P, Zhang L, Li Z, Xu C, Du X, Wu S. Cas12a mediates efficient and precise endogenous gene tagging via MITI: microhomology-dependent targeted integrations. Cell Mol Life Sci. 2020;77:3875-3884. doi:10.1007/s00018-019-03396-8
185. Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316(5827):1039-1043. doi:10.1126/science.1141478
186. Yoon AR, Jung BK, Choi E, Chung E, Hong J, Kim JS, et al. CRISPR-Cas12a with an oAd induces precise and cancer-specific genomic reprogramming of EGFR and efficient tumor regression. Mol Ther. 2020;28(10):2286-2296. doi:10.1016/j.ymthe.2020.07.003
187. Choi E, Hwang H-Y, Kwon E, Kim D, Koo T. Expanded targeting scope of LbCas12a variants allows editing of multiple oncogenic mutations. Mol Ther Nucleic Acids. 2022;30:131-142. doi:10.1016/j.omtn.2022.09.005
188. Huang A, Garraway LA, Ashworth A, Weber B. Synthetic lethality as an engine for cancer drug target discovery. Nat Rev Drug Discov. 2020;19:23-38. doi:10.1038/s41573-019-0046-z
189. Gralewska P, Gajek A, Marczak A, Rogalska A. Participation of the ATR/CHK1 pathway in replicative stress targeted therapy of high-grade ovarian cancer. J Hematol Oncol. 2020;13:39. doi:10.1186/s13045-020-00874-6
190. Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(adp-ribose) polymerase. Nature. 2005;434:913-917. doi:10.1038/nature03443
191. Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917-921. doi:10.1038/nature03445
192. Parrish PCR, Thomas JD, Gabel AM, Kamlapurkar S, Bradley RK, Berger AH. Discovery of synthetic lethal and tumor suppressor paralog pairs in the human genome. Cell Rep. 2021;36(9):109597. doi:10.1016/j.celrep.2021.109597
193. Ryan CJ, Mehta I, Kebabci N, Adams DJ. Targeting synthetic lethal paralogs in cancer. Trends Cancer. 2023;9(5):397-409. doi:10.1016/j.trecan.2023.02.002
194. Mohanraju P, Makarova KS, Zetsche B, Zhang F, Koonin EV, van der Oost J. Diverse evolutionary roots and mechanistic variations of the CRISPR-Cas systems. Science. 2016;353(6299):aad5147. doi:10.1126/science.aad5147
195. Bender G, Yamaci RF, Taneri B. CRISPR and KRAS: a match yet to be made. J Biomed Sci. 2021;28:77. doi:10.1186/s12929-021-00772-0
196. Ma J, Huang L, Hu D, Zeng S, Han Y, Shen H. The role of the tumor microbe microenvironment in the tumor immune microenvironment: bystander, activator, or inhibitor? J Exp Clin Cancer Res. 2021;40:327. doi:10.1186/s13046-021-02128-w
197. Lv B, Wang Y, Ma D, Cheng W, Liu J, Yong T, et al. Immunotherapy: Reshape the Tumor Immune Microenvironment. Front Immunol. 2022;13:844142. doi:10.3389/fimmu.2022.844142
198. Bai R, Cui J. Development of immunotherapy strategies targeting tumor microenvironment is fiercely ongoing. Front Immunol. 2022;13:890166. doi:10.3389/fimmu.2022.890166
199. Liu Z, Shi M, Ren Y, Xu H, Weng S, Ning W, et al. Recent advances and applications of CRISPR-Cas9 in cancer immunotherapy. Mol Cancer. 2023;22(1):35. doi:10.1186/s12943-023-01738-6
200. Lu Y, Xue J, Deng T, Zhou X, Yu K, Deng L, et al. Safety and feasibility of CRISPR-edited T cells in patients with refractory non-small-cell lung cancer. Nat Med. 2020;26(5):732-740. doi:10.1038/s41591-020-0840-5
201. June CH, Sadelain M. Chimeric antigen receptor therapy. N Engl J Med. 2018;379(1):64-73. doi:10.1056/NEJMra1706169
202. Jogalekar M, Rajendran RL, Khan F, Dmello C, Gangadaran P, Ahn B, Ahn B-C. CAR T-cell-based gene therapy for cancers: new perspectives, challenges, and clinical developments. Front Immunol. 2022;13:925985. doi:10.3389/fimmu.2022.925985
203. Tong C, Zhang Y, Liu Y, Ji X, Zhang W, Guo Y, et al. Optimized tandem CD19/CD20 CAR-engineered T cells in refractory/relapsed B-cell lymphoma. Blood. 2020;136(14):1632-1644. doi:10.1182/blood.2020005278
204. Azeez SS, Yashooa RK, Smail SW, Salihi A, Ali AS, Mamand S, et al. Advancing CAR-based cell therapies for solid tumours: challenges, therapeutic strategies, and perspectives. Mol Cancer. 2025;24:191. doi:10.1186/s12943-025-02386-8
205. Eyquem J, Mansilla-Soto J, Giavridis T, van der Stegen SJC, Hamieh M, Cunanan KM, et al. Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature. 2017;543:113-117. doi:10.1038/nature21405
206. Yang C, Liu Y, Huang Z, Liu S, Zhang X, Liu Q, et al. Recent advances and challenges of cellular immunotherapies in lung cancer treatment. Exp Hematol Oncol. 2025;14(1):94.doi:10.1186/s40164-025-00679-8
207. Benjamin R, Graham C, Yallop D, Jozwik A, Mirci-Danicar OC, Lucchini G, et al. Genome-edited, donor-derived allogeneic anti-CD19 chimeric antigen receptor T cells in paediatric and adult B-cell acute lymphoblastic leukaemia: results of two phase 1 studies. Lancet. 2020;396(10266):1885-1894. doi:10.1016/s0140-6736(20)32334-5
208. Guo YL, Tong C, Su L, Zhang W, Jia H, Liu Y, et al. CRISPR/Cas9 genome-edited universal CAR T cells in patients with relapsed/refractory lymphoma. Blood Adv. 2022;6(8):2695-2699. doi:10.1182/bloodadvances.2021006232
209. Dimitri A, Herbst F, Fraietta JA. Engineering the next-generation of CAR T-cells with CRISPR-Cas9 gene editing. Mol Cancer. 2022;21:78. doi:10.1186/s12943-022-01559-z
210. Stadtmauer EA, Fraietta JA, Davis MM, Cohen AD, Weber KL, Lancaster E, et al. CRISPR-engineered T cells in patients with refractory cancer. Science. 2020;367(6481):eaba7365. doi:10.1126/science.aba7365
211. Morris EC, Neelapu SS, Giavridis T, Sadelain M. Cytokine release syndrome and associated neurotoxicity in cancer immunotherapy. Nat Rev Immunol. 2022;22:85-96. doi:10.1038/s41577-021-00547-6
212. Naeem M, Hazafa A, Bano N, Ali R, Farooq M, Razak SIA, et al. Explorations of CRISPR/Cas9 for improving the long-term efficacy of universal CAR-T cells in tumor immunotherapy. Life Sci. 2023;316:121409. doi:10.1016/j.lfs.2023.121409
213. Sterner RM, Sakemura R, Cox MJ, Yang N, Khadka RH, Forsman CL, et al. GM-CSF inhibition reduces cytokine release syndrome and neuroinflammation but enhances CAR-T cell function in xenografts. Blood. 2019;133(7):697-709. doi:10.1182/blood-2018-10-881722
214. Razeghian E, Nasution MKM, Rahman HS, Gardanova ZR, Abdelbasset WK, Aravindhan S, et al. A deep insight into CRISPR/Cas9 application in CAR-T cell-based tumor immunotherapies. Stem Cell Res Ther. 2021;12:428. doi:10.1186/s13287-021-02510-7
215. Gong Y, Klein Wolterink RGJ, Wang J, Bos GMJ, Germeraad WTV. Chimeric antigen receptor natural killer (CAR-NK) cell design and engineering for cancer therapy. J Hematol Oncol. 2021;14:73. doi:10.1186/s13045-021-01083-5
216. Xie G, Dong H, Liang Y, Ham JD, Rizwan R, Chen J. CAR-NK cells: a promising cellular immunotherapy for cancer. eBioMedicine. 2020;59:102975. doi:10.1016/j.ebiom.2020.102975
217. Wang Y, Jin S, Zhuang Q, Liu N, Chen R, Adam SA, et al. Chimeric antigen receptor natural killer cells: a promising antitumor immunotherapy. MedComm (2020). 2023;4(6):e422. doi:10.1002/mco2.422
218. Kong JC, Sa'ad MA, Vijayan HM, Ravichandran M, Balakrishnan V, Tham SK, et al. Chimeric antigen receptor-natural killer cell therapy: current advancements and strategies to overcome challenges. Front Immunol. 2024;15:1384039. doi:10.3389/fimmu.2024.1384039
219. Gurney M, Stikvoort A, Nolan E, Kirkham-McCarthy L, Khoruzhenko S, Shivakumar R, et al. CD38 knockout natural killer cells expressing an affinity-optimized CD38 chimeric antigen receptor successfully target acute myeloid leukemia with reduced effector cell fratricide. Haematologica. 2022;107(2):437-445. doi:10.3324/haematol.2020.271908
220. Daher M, Basar R, Gokdemir E, Baran N, Uprety N, Nunez Cortes AK, et al. Targeting a cytokine checkpoint enhances the fitness of armored cord blood CAR-NK cells. Blood. 2021;137(5):624-636. doi:doi:10.1182/blood.2020007748
221. Morimoto T, Nakazawa T, Matsuda R, Nishimura F, Nakamura M, Yamada S, et al. CRISPR-Cas9-mediated TIM3 knockout in human natural killer cells enhances growth inhibitory effects on human glioma cells. Int J Mol Sci. 2021;22(7):3489. doi:10.3390/ijms22073489
222. Zhang Q, Bi J, Zheng X, Chen Y, Wang H, Wu W, et al. Blockade of the checkpoint receptor TIGIT prevents NK cell exhaustion and elicits potent anti-tumor immunity. Nat Immunol. 2018;19:723-732. doi:10.1038/s41590-018-0132-0
223. Johnston RJ, Comps-Agrar L, Hackney J, Yu X, Huseni M, Yang Y, et al. The immunoreceptor TIGIT regulates antitumor and antiviral CD8+ T cell effector function. Cancer Cell. 2014;26(6):923-937. doi:10.1016/j.ccell.2014.10.018
224. Jo D-H, Kaczmarek S, Shin O, Wang L, Cowan J, McComb S, et al. Simultaneous engineering of natural killer cells for CAR transgenesis and CRISPR-Cas9 knockout using retroviral particles. Mol Ther Methods Clin Dev. 2023;29:173-184. doi:10.1016/j.omtm.2023.03.006
225. Kong R, Liu B, Wang H, Lu T, Zhou X. CAR-NK cell therapy: latest updates from the 2024 ASH annual meeting. J Hematol Oncol. 2025;18:22. doi:10.1186/s13045-025-01677-3
226. Hoerster K, Uhrberg M, Wiek C, Horn PA, Hanenberg H, Heinrichs S. HLA class I knockout converts allogeneic primary NK cells into suitable effectors for “off-the-shelf” immunotherapy. Front Immunol. 2021;11:586168. doi:10.3389/fimmu.2020.586168
227. Mukhopadhyay M. Macrophages enter CAR immunotherapy. Nat Methods. 2020;17(6):561. doi:10.1038/s41592-020-0862-4
228 Chen Y, Yu Z, Tan X, Jiang H, Xu Z, Fang Y, et al. CAR-macrophage: A new immunotherapy candidate against solid tumors. Biomed Pharmacother. 2021;139:111605. doi:10.1016/j.biopha.2021.111605
229. Lu J, Ma Y, Li Q, Xu Y, Xue Y, Xu S. CAR Macrophages: a promising novel immunotherapy for solid tumors and beyond. Biomark Res. 2024;12(1):86. doi:10.1186/s40364-024-00637-2
230. Zhang J, Webster S, Duffin B, Bernstein MN, Steill J, Swanson S, et al. Generation of anti-GD2 CAR macrophages from human pluripotent stem cells for cancer immunotherapies. Stem Cell Reports. 2023;18(2):585-596. doi:10.1016/j.stemcr.2022.12.012
231. Chettri D, Satapathy BP, Yadav R, Uttam V, Jain A, Prakash H. CAR-macrophages: tailoring cancer immunotherapy. Front Immunol. 2025;15:1532833. doi:10.3389/fimmu.2024.1532833
232. Sloas C, Gill S, Klichinsky M. Engineered CAR-macrophages as adoptive immunotherapies for solid tumors. Front Immunol. 2021;12:783305. doi:10.3389/fimmu.2021.783305
233. Siegler EL, Simone BW, Sakemura R, Tapper EE, Horvei P, Cox MJ, et al. Efficient gene editing of CART cells with CRISPR-Cas12a for enhanced antitumor efficacy. Blood. 2020;136(Suppl 1): 6–7. doi:10.1182/blood-2020-141115
234. Chaivorapol C, Beauchesne P, De Jesus R, Dowdle WE, Chen X, Bayley A, et al. Efficient and specific multi-locus editing of allogeneic CAR T cells for hypoimmunity during large scale manufacture using Cas12b. Blood. 2022;140(Suppl 1):1606–1607. doi:10.1182/blood-2022-167627
235. Zhao L, Luo Y, Huang Q, Cao Z, Yang X. Photo-enhanced CRISPR/Cas9 system enables robust PD-L1 gene disruption in cancer cells and cancer stem-like cells for efficient cancer immunotherapy. Small. 2020;16:e2004879. doi:10.1002/smll.202004879
236. Jiang X, Wang J, Deng X, Xiong F, Ge J, Xiang B, et al. Role of the tumor microenvironment in PD-L1/PD-1-mediated tumor immune escape. Mol Cancer. 2019;18:10. doi:10.1186/s12943-018-0928-4
237. Park H, Kang YK, Shim G. CRISPR/Cas9-mediated customizing strategies for adoptive T-cell therapy. Pharmaceutics.2024;16(3):346. doi:10.3390/pharmaceutics16030346
238. Lu Q, Chen R, Du S, Chen C, Pan Y, Luan X, et al. Activation of the cGAS-STING pathway combined with CRISPR-Cas9 gene editing triggering long-term immunotherapy. Biomaterials. 2022;291:121871. doi:10.1016/j.biomaterials.2022.121871
239. Chen B, Mu C, Zhang Z, He X, Liu X. The love-hate relationship between TGF-β signaling and the immune system during development and tumorigenesis. Front Immunol. 2022;13:891268. doi:10.3389/fimmu.2022.891268
240. Fix SM, Forget M-A, Sakellariou-Thompson D, Wang Y, Griffiths TM, Lee M, et al. CRISPR-mediated TGFBR2 knockout renders human ovarian cancer tumor-infiltrating lymphocytes resistant to TGF-β signaling. J Immunother Cancer. 2022;10(7):e003750. doi:10.1136/jitc-2021-003750
241. Tang N, Cheng C, Zhang X, Qiao M, Li N, Mu W, et al. TGF-β inhibition via CRISPR promotes the long-term efficacy of CAR T cells against solid tumors. JCI Insight. 2020;5(4):e133977. doi:10.1172/jci.insight.133977
242. Haake M, Haack B, Schäfer T, Harter PN, Mattavelli G, Eiring P, et al. Tumor-derived GDF-15 blocks LFA-1 dependent T cell recruitment and suppresses responses to anti-PD-1 treatment. Nat Commun. 2023;14(1):4253. doi:10.1038/s41467-023-39817-3
243. He L, Li Z, Su D, Du H, Zhang K, Zhang W, et al. Tumor microenvironment-responsive nanocapsule delivery CRISPR/Cas9 to reprogram the immunosuppressive microenvironment in hepatoma carcinoma. Adv Sci (Weinh). 2024;11(26):e2403858. doi:10.1002/advs.202403858
244. Sorrentino C, D'Antonio L, Ciummo SL, Fieni C, Landuzzi L, Ruzzi F, et al. CRISPR/Cas9-mediated deletion of Interleukin-30 suppresses IGF1 and CXCL5 and boosts SOCS3 reducing prostate cancer growth and mortality. J Hematol Oncol. 2022;15(1):145. doi:10.1186/s13045-022-01357-6
245. Sorrentino C, Ciummo SL, D'Antonio L, Fieni C, Lanuti P, Turdo A. Interleukin-30 feeds breast cancer stem cells via CXCL10 and IL23 autocrine loops and shapes immune contexture and host outcome. J Immunother Cancer. 2021;9(10):e002966. doi:10.1136/jitc-2021-002966
246. D'Antonio L, Fieni C, Ciummo SL, Vespa S, Lotti L, Sorrentino C, et al. Inactivation of interleukin-30 in colon cancer stem cells via CRISPR/Cas9 genome editing inhibits their oncogenicity and improves host survival. J Immunother Cancer. 2023;11(3):e006056. doi:10.1136/jitc-2022-006056
247. Ma S, Li Y, Liu F, Wang X, Qin Z, Wang L, et al. Hierarchical-unlocking virus-esque NanoCRISPR precisely disrupts autocrine and paracrine pathway of VEGF for tumor inhibition and antiangiogenesis. J Control Release. 2024;366:505-518. doi:10.1016/j.jconrel.2024.01.001
248. Hariprabu KNG, Sathya M, Vimalraj S. CRISPR/Cas9 in cancer therapy: a review with a special focus on tumor angiogenesis. Int J Biol Macromol. 2021;192:913-930. doi:10.1016/j.ijbiomac.2021.10.029
249. Dey P, Kimmelman AC, DePinho RA. Metabolic codependencies in the tumor microenvironment. Cancer Discov.2021;11(5):1067-1081. doi:10.1158/2159-8290.CD-20-1211
250. Ma K, Mao Q, Fei B, Ni T, Zhang Z, Ni H. Metabolic reprogramming and immune microenvironment characteristics in laryngeal carcinoma: advances in immunotherapy. Front Immunol. 2025;16:1589243. doi:10.3389/fimmu.2025.1589243
251. Huang Y, Qin G, Cui T, Zhao C, Ren J, Qu X. A bimetallic nanoplatform for STING activation and CRISPR/Cas mediated depletion of the methionine transporter in cancer cells restores anti-tumor immune responses. Nat Commun. 2023;14(1):4647. doi:10.1038/s41467-023-40345-3
252. Leibowitz ML, Papathanasiou S, Doerfler PA, Blaine LJ, Sun L, Yao Y, et al. Chromothripsis as an on-target consequence of CRISPR-Cas9 genome editing. Nat Genet. 2021;53(6):895-905. doi:10.1038/s41588-021-00838-7
253. Aussel C, Cathomen T, Fuster-Garcia C. The hidden risks of CRISPR/Cas: structural variations and genome integrity. Nat Commun. 2025;16(1):7208. doi:10.1038/s41467-025-62606-z
254. Tang XZE, Tan SX, Hoon S, Yeo GW. Pre-existing adaptive immunity to the RNA-editing enzyme Cas13d in humans. Nat Med. 2022;28(7):1372-1376. doi:10.1038/s41591-022-01848-6
255. Charlesworth CT, Deshpande PS, Dever DP, Camarena J, Lemgart VT, Cromer MK, et al. Identification of preexisting adaptive immunity to Cas9 proteins in humans. Nat Med. 2019;25(2):249-254. doi:10.1038/s41591-018-0326-x
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Lirenhui Zhou, Meiya Mu, Meihua Yang, Xiaojing Liu, Guangrong Zou, Chaoxing Liu

This work is licensed under a Creative Commons Attribution 4.0 International License.
Copyright
Authors publishing in Cancer Biome and Targeted Therapy retain full copyright of their work. By submitting a manuscript, authors grant the publisher (GCINC Press) a non-exclusive license to publish, distribute, and archive the article, and to identify itself as the original publisher.
License
All articles are published open access under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0).
https://creativecommons.org/licenses/by/4.0/. This license permits unrestricted use, distribution, reproduction, and adaptation in any medium, including for commercial purposes, provided that:
- Proper attribution is given to the original author(s) and source,
- A link to the license is provided, and
- Any changes made are clearly indicated.
Author Rights
Authors retain the right to:
- Use their article in future works (e.g., books, theses, lectures)
- Share and archive the final published version on institutional repositories or personal websites
- Adapt or translate their work, or authorize others to do so, with proper citation
Reuse by Third Parties
Content is licensed under the Creative Commons Attribution 4.0 International License (CC BY 4.0). Third parties may copy, redistribute, remix, transform, and build upon the material for any purpose, including commercial use, provided that appropriate credit is given to the original author(s).
Archiving and Preservation
All articles are made freely available immediately upon publication, without embargo. Cancer Biome and Targeted Therapy is hosted on the Open Journal Systems (OJS) platform, developed by the Public Knowledge Project (PKP). The journal participates in long-term digital preservation through the PKP Preservation Network (PKP PN) using the LOCKSS system. Authors are encouraged to self-archive in institutional repositories, disciplinary archives, and preprint servers in accordance with the license terms.